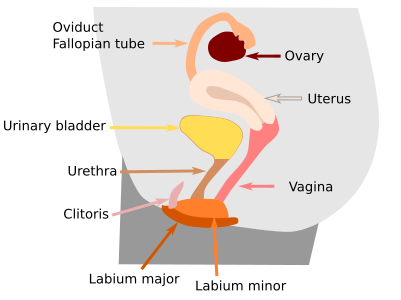
The female reproductive system produces egg cells, the female gametes. In mammals, if fertilization happens, the embryo is implanted in the female reproductive ducts, where posterior development occurs until birth. The physiology of the female reproductive system is different depending on whether there is fertilization or not. Several components of the female reproductive system can be distinguished: ovaries (or female gonads), reproductive ducts, and external genitalia (Figures 1 and 2).
1. Ovary
Ovaries perform two main functions: the production of gametes (egg cells) and hormones like estrogens and progestagens (a family of hormones where progesterone is included), which are steroid hormones. Ovaries are a pair of organs located in the pelvic cavity, on both sides of the uterus. Although their shape changes during the menstrual cycle, they are usually ovoids, and in humans, they are 3–4 cm long, 1.5 cm wide, and 1 cm thick.
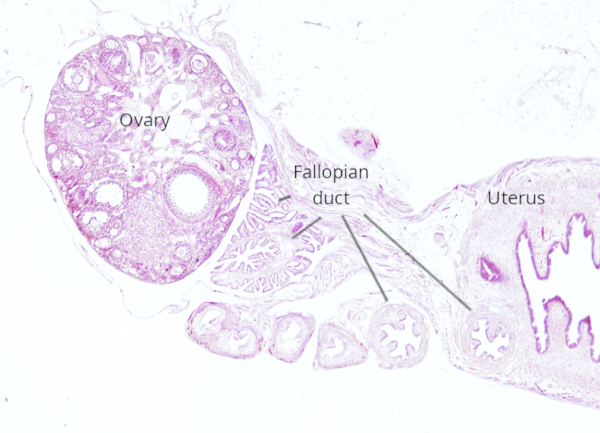
Each ovary is divided into the ovarian surface epithelium, tunica albuginea, cortical region, and medullary region. The surface epithelium is the outermost layer of the ovary, made up of cuboidal or squamous cells derived from the visceral peritoneum (mesothelium). The tunica albuginea is a layer of dense connective tissue found immediately beneath the surface epithelium. The ovarian cortex comes next. It is a more or less compact stroma containing ovarian follicles in different developmental stages. Each ovarian follicle is composed of somatic cells wrapping an oocyte. The oocytes produced during embryonic development and arrested in meiotic prophase I are stored in the cortex. In each menstrual cycle, one or several of these arrested follicles restart meiosis, and the follicle develops. Surrounded by the cortex, the ovarian medulla is found in the inner part of the ovary, although it is difficult to find a clear limit between the medulla and cortex. The ovarian medulla is fibro-elastic tissue with abundant blood vessels and nerves, both entering and leaving the ovary through the hilum. There are no ovarian follicles in the medulla.
In humans, each ovary is attached to other structures by so-called ligaments. The upper part of the ovary is attached to the peritoneum, the wall of the pelvis, by the suspensory ligament. The posterior portion of the broad ligament of the uterus forms the mesovarium, which also supports the ovary. Through these last two ligaments, nerves and blood vessels enter and leave the ovary. The lower part of the ovary is attached to the uterus by the utero-ovarian or ovarian ligament.
Oocytes are produced from oogonia, the female germinal cells, during the embryonary period. Oogonia are derived from germinal cells before the gonadal ridges develop into the gonads in the embryo. There is an initial period of proliferation by mitosis that yields about 5 to 7 million oogonia. In humans, during the sixth month of fetal development, proliferation stops and oogonia become primary oocytes by meiosis. The meiotic process is arrested in prophase I. That is, before the first meiotic division. Arrested oocytes are distributed in the outer part, or cortex, of the developing ovary. They remain arrested in this location until maturation starts during the first menstrual cycle. Meiosis is restarted only for those oocytes to be released during each ovulation. In humans, the second meiotic division only starts if fertilization takes place.
Ovarian follicles are made up of somatic cells and one oocyte. The somatic cells are form the environment for proper oocyte development. The size of an ovarian follicle is indicative of the stage of the development of the oocyte. The maturation process of the follicles is divided morphologically into three stages: primordial, growing (primary, secondary, and tertiary follicles), and mature (Graaf follicles).
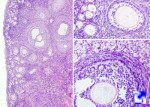
Primordial follicles are found just beneath the tunica albuginea. They are one cell-thick layer of somatic cells wrapping one oocyte, which is arrested in prophase I. Somatic cells are rather flat to cuboidal, in close apposition to the oocyte. The follicle is separated from the surrounding stroma by a basal lamina.
Those follicles that start growing also begin to mature and will eventually release a fully developed egg cell (ovum) during ovulation at the end of this maturing process. Depending on the author and the developing stage, follicles are named specifically. Primary follicles show an increase in the size of the oocyte, and the follicle somatic cells wrapping the oocyte change from flattened to cuboidal shapes. Furthermore, the zona pellucida starts to be visible between the oocyte and the somatic cells. As maturation progresses, follicle somatic cells proliferate and are arranged into several layers, known as the granulosa layer. Granulosa cells are enclosed by the follicle basement membrane, or basal membrane. Stroma cells surrounding the follicle reorganize and wrap the basal membrane to form a multi-layered sheath made up of somatic flattened cells known as theca. The theca may become thick, and an internal and an external part can be distinguished. During the process, besides growing in size, the oocyte has matured by reorganizing the cytoplasm, storing cortical granules below the cell membrane, forming microvilli, and making other cell changes. Secondary follicles, or antral follicles, develop a cell-free space among the granulosa cells. This space is the antrum, and it is formed when granulosa cell proliferation reaches around 5 layers of cells. Now, the oocyte stops growing. However, follicle somatic cells keep proliferating, and the follicle gets bigger, including the antrum. The oocyte is separated from the granulosa, but a group of granulosa cells remain covering the oocyte. These granulosa cells and the oocyte are now isolated from the rest of the granulosa cells in the antrum, except for a bridge of granulosa cells known as discus proligerus or cumulus oophorus. These somatic cells around the oocyte will later, during ovulation, form the corona radiata.
The mature follicle, or Graaf follicle, is so big that it pushes the ovarian tunica albuginea outward. The antrum takes almost all the inner follicular space, and the oocyte, with its surrounding somatic cells of corona radiata, is disconnected from granulosa cells just before the ovulation. Theca cells are now well-developed. Both theca and granulosa cells release androgen and estrogen hormones, respectively. After stimulation by luteinizing hormone released by the hypophysis, the oocyte restarts meiosis and undergoes the first meiotic division to become a secondary oocyte. It is in this stage that the oocyte is released from the follicle, a process known as ovulation.
After the egg cell has been released, the follicle somatic cells become the corpus luteum. They produce progesterone and estrogens that stimulate the cells that form the uterus walls so that embryo implantation can take place. If there is no fertilization, the corpus luteum degenerates several days after ovulation. If fertilization happens, the corpus luteum grows and continues to release progesterone and estrogens, mainly during the first weeks of the pregnant period.
2. Oviducts
Egg cells released during ovulation are collected in the fallopian tube, also known as the uterine tube, which leads them to the uterus. There are two fallopian tubes, one per ovary. In humans, they are 10 to 12 cm long. Fertilization and part of the early embryonic development take place inside the fallopian tubes. The embryo arrives at the uterus during the blastocyst stage, when implantation occurs. Sperm cells need to swim a long way, including the uterus wall and a long portion of the fallopian tubes, before they contact the egg cell.
The fallopian tube is divided into several parts. The infundibulum, or pavilion, is close to the ovary, has a funnel-like shape, and fetches the egg cell immediately after ovulation. The longest part of the Fallopian tube is theampullary region, which is about two-thirds of the total length. Fertilization occurs in this segment. The isthmus is near the uterus and is the narrower part of the fallopian tube. The interstitial, or intramural, part of the fallopian tube enters the walls of the uterus and connects with the internal cavity of the uterus.
The wall of the fallopian tubes is surrounded by a serous layer, or visceral peritoneum, made up of mesothelium and a thin layer of connective tissue. Toward the lumen, there is a layer of smooth muscle divided into a longitudinal external layer and a thicker circular internal layer. In contact with the lumen, there is a mucosa layer with longitudinal folds protruding into the lumen. The mucosa is made up of connective tissue and a simple columnar epithelium with two types of cells, ciliated and non-ciliated. The movement of ciliapropels the egg cell toward the uterus. Non-ciliated cells are secretory cells that release nutritious substances for the egg cell. The proportion of these types of cells changes during the menstrual cycle. Estrogens promote more ciliated cells and an increase in cellular height. The egg cell cannot move by itself, so it is propelled by ciliated cells and the peristaltic movements of the fallopian tubes. Sperm cells travel in the opposite direction, toward the ovary. Besides the power of the flagellum, it is not known what mechanism pushes sperm cells through fallopian tubes to meet the egg cell.
The uterus is the compartment of the reproductive ducts where most embryonary development takes place. It is found between the fallopian tubes and the vagina. In humans, it is around 7.5 cm long. The uterus is divided into a superior part, or body, and an inferior part, or cervix. The wall of the uterus is thick and divided into three layers: the endometrium, or uterus mucosa, is a layer composed of simple columnar epithelium and connective tissue; the myometrium, or muscle layer, is continuous with the muscle of the fallopian tubes; and the perimetrium, which is the peritoneal layer. The endometrium and myometrium undergo major changes during menstrual cycles. If fertilization takes place, the embryo attaches to the endometrium (implantation) and eventually invades the uterus wall to form the placenta. The placenta is composed of two components: the chorion, derived from the embryo, and the decidua, derived from the endometrium layer. The mucosa of the cervix is morphologically different because it has exocrine glands that release more or less dense mucous substances according to the point of the menstrual cycle, facilitating or inhibiting the entrance of sperm cells in the uterus lumen.
The vagina is the receptacle for the male sexual organ and communicates the uterus with the vestibule of the vulva, which is the part of the vulva located between the two labia minora. The vaginal wall is formed of a thin mucosa with a stratified, usually keratinized, squamous epithelium. Below, there is a layer of smooth muscle divided into two sublayers, one circular and one longitudinal. The longitudinal one is thicker, and it is continuous with the muscle layer of the uterus. There is striated muscle in the part of the vagina near the exterior of the body. Wrapping the muscle layer, there is an adventitia layer of dense connective tissue, and then loose connective tissue. The vagina does not contain glands, and its lubrication is caused by the secretion of glands located in the cervix of the uterus. The external lubrication of the vaginal entrance is produced by glands located between the labia of the vulva.
3. External genitalia
The vulva is the external female reproductive organ. It includes the mons pubis, labia major, labia minor, clitoris, and the vulva vestibule. Mons pubis is a rounded elevation produced by subcutaneous adipose tissue. Labia are cutaneous folds with sweat and sebaceous glands. The external labia (labia major) have hair follicles and smooth muscle. Clitoris is an erectile structure homologous to the penis, with cavernous bodies and a clitoral glans (hood). The vulvar vestibulus is covered by stratified squamous epithelium with many small mucous glands and other more complex tubule-alveolar glands that release their content into the vaginal opening. These glands lubricate the external part of the female external organ. The external genitalia contain many touch and pressure sensory receptors, like Meissner corpuscles, Pacini corpuscles, and free-ending axons.
 Reproductive
Reproductive 